Featured Care Partner
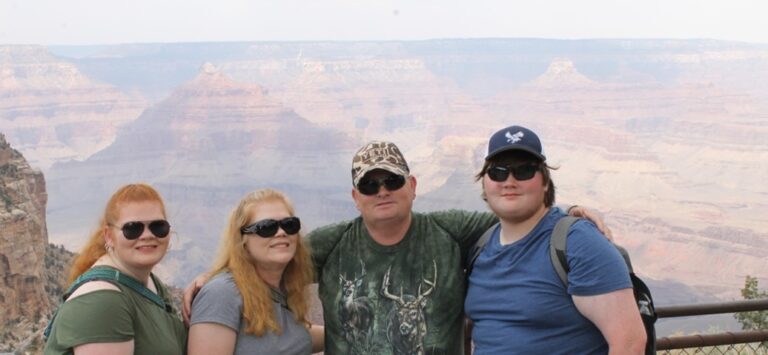
Care Partner Corner Features The Jett Family
By Tamela Jett
Imagine. Just for a moment. This moment. No preparation. You are instantly in a different country, a new one. One that speaks a different language from you. Your ability to communicate is limited. Conversations are going on around you, but you don’t understand the language. You want to be a part of the conversation, but you don’t speak the language. You want to read the words that are written around you, maybe it’s even a lunch menu. You can’t read the language. You want to write something, anything with words, but you are unable to write in that language. This is the analogy I give when I describe James’s aphasia. He has Global Aphasia. James has trouble understanding all of your words. He also has trouble finding the right words.
The irony in my analogy – James was in another country. He was working for Cisco Systems at the 2016 Olympic Games in Rio de Janeiro, Brazil as a project manager. He had just finished a thirty day stay, and after a short break at home, had returned for the Para Olympic Games. After suffering a few days from severe headaches James lost the ability to communicate. At first, James was diagnosed with encephalitis. It was a few days later that we learned James had two mini-strokes. I depended on his co-workers and the SOS nurses to keep me up to date. While hospitalized, our phone conversations consisted of James playing songs. Conversations were limited to guessing games of single words. There were so many unknowns with him being far away. Cisco was prepared to fly me to Brazil. An SOS nurse advised me to stay home and get things ready for James. That was smart advice. The struggle to get James back to the States is a story for another day, but it did include a doctor flying back to the States with James.
I had so much love and support from my family, friends, and coworkers from the moment I received the call. That life changing call. Each day I did my best to keep my emotions in check while in the classroom and at home around the children. One of my confessions during those days before James came home is this, one night I sat on my bedroom floor and called my daddy. I told him that I just needed someone to talk to who wasn’t going to cry. I knew the lives of my family would never be the same. I didn’t want someone else telling me everything was going to be okay because at that moment, things weren’t okay. I needed someone that would talk to me in real terms. I wanted truths to my new reality. My new normal.
When James started seeing the neurologists, they would keep the conversations quick and simple. I had to ask the questions in order to get answers that I really already knew from my own research, but was hoping didn’t apply to James. I just hoped – just needed- to hear that the area in James’s brain that was damaged from the stroke, would one day heal and everything would go back to the way it was. That’s not how aphasia works. Instead, I was told that he would “keep getting better.” I knew this. It is true. It gets better. Not overnight but gradually.
Immediate therapy is critical. Those first 12 weeks. This is what I had been told and read. Over and Over. What James would learn in those first 12 weeks would be the bulk of his learning, but he would continue to relearn for the rest of his life. Yet, James did not start speech therapy right away. My mind kept ticking off the days as I knew he was missing out on important relearning opportunities. A retired speech therapist from the school I taught took a class on aphasia. Just for me. Just for James. For us. She shared with me websites and apps. If James couldn’t start speech right away, I was determined to start him on a program at home. I purchased the Tactus App. It was that experience that gave me a true picture of the severity of the damage from the strokes. It was also that app that began to help him improve his literacy skills. He was able to work on it at home, while I was at work.
Life lessons. PSAs. These are lessons that I have learned that may help others.
Finances. One of my stressors was the worry of our finances. With our youngest in middle school and our oldest in high school, how were we going to keep the lifestyle we were used to? I won’t lie. I was worried about how we were going to be able to afford our home without his income. James had taken out a long term disability insurance policy. This policy is in effect until he is 65 and supplements the Social Security Disability. Smart planning, James.
Body parts. Don’t laugh. This is important. Some of the first vocabulary to teach your loved one with aphasia is body parts and the types of aches and pains. Practice those words with pictures or videos. Who would have thought that simple song, “Heads, Shoulders, Knees, and Toes” would be such an important song in communicating?
Passwords. Know your loved one’s passwords that are important to your household. James’s fingers had muscle memory. He was able to type passwords to his accounts. His fingers moved fast across the keys. If he slowed down, he would not have been able to type the passwords. I would stand over his hands as he would retype often so I could get them written.
Support. It has been important for James to be able to connect with others with aphasia. We have been so thankful of all the support the USC Aphasia Lab has offered. It helps to know that we are not alone. If friends offer help, take it. As a caregiver, mental breaks are necessary. As a stroke survivor with aphasia, they need to be a part of the outside world.
Mental Health Counselors. If I had it to do over, I would have taken my children to counseling. I watched them closely for behavioral changes. I worked hard to keep things as normal for them as possible. I could spend a few extra pages bragging about the great children James and I have raised. You wouldn’t know that they have experienced a type of trauma in their lives (or so I thought). Three years after aphasia had become part of our daily lives, I watched our daughter practice a monologue she had written for a state high school theatrical competition about her experience. It hurt to watch.
Restaurants. Really? Restaurants. Oh, yes. My PSA is this – look at the menu BEFORE going to the restaurant or drive thru. Talk about it and pull up pictures. Make semi-decisions on food choices before setting out. You’re welcome.
Communication. Have you seen the coach that blows his whistle and makes the letter T sign with his hands? James and I don’t use it as often as we could/should, but when we use it, it is highly effective. When one of us uses that symbol, we both stop the conversation, slow down, and start over. It is understood that the time out is not because we are angry, it is because we are confused by the conversation or what was said was misunderstood.
One of the first phrases James began to say after his stroke was “God has a plan.” He does. God has a plan for James and our family. I am amazed at how far James has come. It didn’t all happen in the first 12 weeks, but James does do or say something that surprises me almost every day. We go to church. We take vacations and go on outings. James is involved in his hobbies, and I’m involved in mine. Our children – we couldn’t be more proud. Life with aphasia has created a new norm for us. Five years later, I am still calling it our new norm. Life with aphasia – we are okay. We are going to be okay.
Former Featured Care Partners

Tell us your story. How did you become a caregiver/support partner for someone with aphasia?
On May 1, 2015 my husband had a stroke. I was out of town and when I arrived at the hospital several hours later he could not talk and his right side was paralyzed. It was a dark and scary time. We didn’t know what to expect.
What kind of changes took place in your lives as a result of your loved one having a stroke and aphasia?
There was an immediate need to contact his employer, arrange for disability, fill out forms, and contact friends and loved ones. This was hard to manage when your world is all of a sudden upside down and you are in a daze. Later changes involved me taking over all the finances, insurance matters, continuing to update friends and family and be sure my husband was taken care of and appointments were attended. More changes came when he was forced to retire because of his stroke and we started over by selling our house in Maryland and moving to South Carolina.
What helped you and your loved one the most as you navigated your “new normal” after a stroke?
Prayer. And friends. People brought meals. Friends helped clean the house. Neighbors helped and supported us. Getting into therapy as early as possible is key.
What do you know now that you wished you had known right after your loved one had a stroke and aphasia?
To get into aggressive therapy ASAP at an inpatient rehab hospital – speech therapy, physical therapy and occupational therapy. That someone would have told us about Aphasia on day 1 or 2. We didn’t even hear the word Aphasia until he was in outpatient therapy a month after his stroke.
How did you help other family members and friends understand aphasia and how it affected your loved one?
By explaining it was his speech that was affected, not his cognitive abilities. And to speak in a normal tone of voice, no need to yell. And even though he could not verbalize his thoughts, he knew what you were saying.
What advice do you have for other caregivers/support partners of someone experiencing aphasia?
Listen. Be patient. Let your loved one be involved in speaking to other people and let your loved one talk.
Is there anything else you would like to share about your experience?
Neither of us would have signed up for this, but it has been a growing and stretching experience for each of us in different ways. It has drawn us closer to each other and to God. We have made some amazing friends and wouldn’t trade this for anything.
We were tipped off our axis catapulted into another sphere to learn a language foreign to us beginning August 8, 2016 when my husband had an ischemic stroke. Life as we knew it shattered!
My wife role changed. Suddenly I became protector, caregiver, supporter, cheerleader for my love and life companion.
Focused on recovery we laid aside things that pulled us away from first priority of learning to live well within the circumstances of stroke survival. We have experienced continuing progress through these ‘after years’. It would have been encouraging to hear that the rate of forward progression may change, but it can continue beyond the one year /eighteen-month time marker.
Sorting through the broken life, keeping salvageable parts while discarding others led us into a new adventure of educating family and friends of changes through conversations, text messages, sharing USC Aphasia Lab Facebook posts, and at first brief interactions that eventually led to good visits.
Following the unfortunate norm some people shy away because they don’t understand how to interact in the new lifescape we are creating. However, because we researched, reached out and explored every available avenue for improvement and recovery we have gained a new ever growing circle of friends and professionals. We would encourage other stroke survivor families to reach out and learn from each other’s experiences as you recreate the life you now have. Life is different, but it can still be rewarding.
Daily life can be very frustrating at times. I have learned to be present in the moment, give thanks for the Lord’s mercies that are new every morning, and let the day flow with grace. Reminding myself to be patient I smile and with a heart filled with gratitude I thank my God for the privilege of sharing life together.
Van and Dee have been married 54 years and they look forward to sharing many more anniversaries together.

My daughter Megan, a 37-year old mother of two with a promising career, who was always involved in charitable events, and helping friends in need, had a stroke and resulting brain aneurysm while on vacation four hours from home. She was airlifted to a trauma hospital where she had surgery to coil the aneurysm and a craniotomy to remove a large blood clot. When I first saw her after the surgery I cried harder than I have ever cried in my life. I knew what to expect. My father had a very similar situation when Megan was a one-year old child. He lived for two years after his stroke, but was never able to talk to us again after his stroke. The inability to communicate was frustrating for him and heartbreaking for me. I fully expected Megan to follow suit. I know now the value of immediate and intense therapy.
I immediately knew that I would quit my job and take care of her and her children. I would be her caregiver for as long as I could. No question. For four weeks I sat by her side in the hospital and worried what she was thinking as she lay there. Was she wondering where she was, what had happened and where her children were? She has since told me she didn’t remember thinking anything. It now makes sense to me. She had no memory, so there was nothing to wonder or think about.
As time passed, she began to show improvement. She had her feeding tube removed and could now eat. She also walked with a walker with help from her therapist, but still could not verbalize her words, which caused her to remain silent most of the time. When she was well enough, I had her transported to a rehab hospital in Columbia. The most important thing was for her to see her children and for her children to see her. I needed to be home and to go back to work.
The intense therapy she received did wonders! When she was released from inpatient care, we made the trip from Chapin to Columbia several times a week for therapy as long as her insurance allowed outpatient coverage. It was there she met Ms. Mary. Ms. Mary gave us information about the Aphasia Lab at USC. I put it aside. I was so busy taking care of my house, her house, my grandchildren and working, I couldn’t even think about it at that time.
When outpatient therapy ended, I could tell Megan needed something more. She needed interaction. She had been such an “involved” person before this, that not doing anything would not work for her. She couldn’t drive, and didn’t feel comfortable enough to have friends over because of the aphasia. In fact, she would tell me to say no to anyone that wanted to come over. The aphasia kept her somewhat in isolation for quite a while. That is when I reached out to Dr. Spell. Megan is now gaining her confidence when talking to people, ordering in restaurants and being with her friends. She still does not like to be in a large group of people because of some hearing loss, but I get the feeling she is content. I see a much happier Megan.
Before the stroke, whenever I needed to talk, or had something I didn’t really know how to handle, Megan would always say “I got this Mom”. Then the day came when it was my time to say said “I got this Megan”. Over time my role as caregiver has evolved into mostly taking care of her finances, read and respond to her mail, emails, and phone calls. I interact with schools, doctors and dentists for the family. I carry a Power of Attorney with me everywhere I go.
I believe that my patience and her impatience created the perfect combination to get to our “new normal”. I would have taken care of everything for her as long as I had a breath, but her impatience set in and she now does most things on her own. I feel like my baby girl has grown up for a second time.
Care Partner Resources
For a free Aphasia Caregiver Guide, go to the National Aphasia Association’s (NAA) site to download your copy: https://www.aphasia.org/aphasia-resources/aphasia-caregiver-guide/
In this guide, the NAA provides helpful information about aphasia, recovery and how you and your loved one can navigate all that goes with the recovery process. Some of the suggested support organizations included in this guide are listed below. Neither the NAA nor the University of South Carolina Aphasia Lab officially endorse any of these organizations, but all are potentially useful resources.
Caregiver Action Network
http://caregiveraction.org/
“Caregiver Action Network is the nation’s leading family caregiver organization working to improve the quality of life for the more than 90 million Americans who care for loved ones with chronic conditions, disabilities, disease, or the frailties of old age.”
Caregiver Support Services
http://caregiversupportservices.com/
“Caregiver Support Services (CSS) is a non-profit organization with a 501(c) (3) tax-exempt status. CSS was founded in 1997 by Terrence and Eboni Green, a husband and wife team, after the couple recognized that most individuals who provide care for a loved one or client do not know where to start when it comes to gathering and coordinating resources and services.”
Family Caregiver Alliance
https://www.caregiver.org/
“Founded in the late 1970s, Family Caregiver Alliance is the first community-based nonprofit organization in the country to address the needs of families and friends providing long-term care for loved ones at home. FCA, as a public voice for caregivers, shines light on the challenges caregivers face daily and champions their cause through education, services, and advocacy. The services, education programs, and resources FCA provides are designed with caregivers’ needs in mind and offer support, tailored information, and tools to manage the complex demands of caregiving.”
National Alliance for Caregiving
http://www.caregiving.org/
“Established in 1996, the National Alliance for Caregiving is a non-profit coalition of national organizations focusing on advancing family caregiving through research, innovation, and advocacy. The Alliance conducts research, does policy analysis, develops national best-practice programs, and works to increase public awareness of family caregiving issues.”

